Can Swallowing A Can Tab Kill You
Pain
Definition
Pain is an unpleasant feeling that is conveyed to the brain by sensory neurons. The discomfort signals actual or potential injury to the body. Withal, pain is more than a sensation, or the physical sensation of hurting; information technology also includes perception, the subjective estimation of the discomfort. Perception gives information on the pain'southward location, intensity, and something about its nature. The various conscious and unconscious responses to both sensation and perception, including the emotional response, add further definition to the overall concept of pain.
Description
Hurting arises from any number of situations. Injury is a major cause, only pain may too arise from an affliction. It may accompany a psychological condition, such as depression, or may fifty-fifty occur in the absence of a recognizable trigger.
Acute hurting
Acute pain ofttimes results from tissue damage, such every bit a skin burn or broken os. Astute pain tin also be associated with headaches or muscle cramps. This blazon of pain usually goes away as the injury heals or the cause of the pain (stimulus) is removed.
To understand acute pain, it is necessary to understand the nerves that support it. Nerve cells, or neurons, perform many functions in the body. Although their full general purpose, providing an interface betwixt the encephalon and the body, remains constant, their capabilities vary widely. Certain types of neurons are capable of transmitting a pain indicate to the encephalon.
As a grouping, these pain-sensing neurons are chosen nociceptors, and virtually every surface and organ of the body is wired with them. The central part of these cells is located in the spine, and they send threadlike projections to every function of the trunk. Nociceptors are classified according to the stimulus that prompts them to transmit a pain bespeak. Thermoreceptive nociceptors are stimulated by temperatures that are potentially tissue damaging. Mechanoreceptive nociceptors reply to a pressure stimulus that may cause injury. Polymodal nociceptors are the near sensitive and can respond to temperature and pressure. Polymodal nociceptors besides reply to chemicals released by the cells in the area from which the pain originates.
Nerve cell endings, or receptors, are at the front end of hurting sensation. A stimulus at this function of the nociceptor unleashes a cascade of neurotransmitters (chemicals that transmit information within the nervous system) in the spine. Each neurotransmitter has a purpose. For example, substance P relays the pain bulletin to nerves leading to the spinal cord and brain. These neurotransmitters may also stimulate nerves leading back to the site of the injury. This response prompts cells in the injured area to release chemicals that not merely trigger an immune response, but likewise influence the intensity and duration of the pain.
Chronic and aberrant pain
Chronic pain refers to pain that persists after an injury heals, cancer pain, pain related to a persistent or degenerative disease, and long-term pain from an unidentifiable cause. Information technology is estimated that 1 in three people in the United States will feel chronic hurting at some point in their lives. Of these people, approximately fifty million are either partially or completely disabled.
Chronic pain may exist caused by the trunk'south response to acute pain. In the presence of continued stimulation of nociceptors, changes occur within the nervous system. Changes at the molecular level are dramatic and may include alterations in genetic transcription of neurotransmitters and receptors. These changes may as well occur in the absence of an identifiable crusade; one of the frustrating aspects of chronic hurting is that the stimulus may be unknown. For example, the stimulus cannot be identified in equally many as 85% of individuals suffering lower back pain.
Scientists have long recognized a human relationship betwixt depression and chronic pain. In 2004, a survey of California adults diagnosed with major depressive disorder revealed that more than than half of them also suffered from chronic pain.
Other types of abnormal pain include allodynia, hyperalgesia, and phantom limb pain. These types of pain ofttimes arise from some damage to the nervous system (neuropathic). Allodynia refers to a feeling of hurting in response to a commonly harmless stimulus. For example, some individuals who have suffered nervus impairment equally a result of viral infection experience unbearable pain from just the light weight of their clothing. Hyperalgesia is somewhat related to allodynia in that the response to a painful stimulus is farthermost. In this case, a mild pain stimulus, such every bit a pin prick, causes a maximum pain response. Phantom limb pain occurs after a limb is amputated; although an private may exist missing the limb, the nervous organization continues to perceive pain originating from the area.
Causes and symptoms
Hurting is the near common symptom of injury and disease, and descriptions can range in intensity from a mere ache to unbearable agony. Nociceptors have the ability to convey information to the brain that indicates the location, nature, and intensity of the hurting. For instance, stepping on a blast sends an data-packed message to the encephalon: the human foot has experienced a puncture wound that hurts a lot.
Pain perception besides varies depending on the location of the pain. The kinds of stimuli that crusade a pain response on the skin include pricking, cutting, crushing, burning, and freezing. These same stimuli would non generate much of a response in the intestine. Intestinal pain arises from stimuli such as swelling, inflammation, and distension.
Diagnosis
Pain is considered in view of other symptoms and private experiences. An observable injury, such as a cleaved bone, may be a clear indicator of the type of hurting a person is suffering. Determining the specific crusade of internal pain is more than difficult. Other symptoms, such as fever or nausea, help narrow downwardly the possibilities. In some cases, such as lower back pain, a specific cause may not be identifiable. Diagnosis of the disease causing a specific pain is further complicated by the fact that pain can be referred to (felt at) a skin site that does non seem to be connected to the site of the hurting's origin. For example, pain arising from fluid accumulating at the base of the lung may be referred to the shoulder.
Since pain is a subjective experience, it may be very difficult to communicate its exact quality and intensity to other people. There are no diagnostic tests that can determine the quality or intensity of an individual'southward pain. Therefore, a medical examination will include a lot of questions almost where the pain is located, its intensity, and its nature. Questions are also directed at what kinds of things increase or save the hurting, how long it has lasted, and whether there are whatsoever variations in it. An private may exist asked to utilize a pain calibration to describe the hurting. One such scale assigns a number to the pain intensity; for example, 0 may point no hurting, and 10 may indicate the worst pain the person has ever experienced. Scales are modified for infants and children to adjust their level of comprehension.
Treatment
In that location are many drugs aimed at preventing or treating pain. Nonopioid analgesics, narcotic analgesics, anticonvulsant drugs, and tricyclic antidepressants work by blocking the production, release, or uptake of neurotransmitters. Drugs from different classes may be combined to handle certain types of pain.
Nonopioid analgesics include common over-the-counter medications such as aspirin, acetaminophen (Tylenol), and ibuprofen (Advil). These are most often used for pocket-sized pain, but there are some prescription-strength medications in this class.
Narcotic analgesics are only bachelor with a doctor's prescription and are used for more severe pain, such equally cancer pain. These drugs include codeine, morphine, and methadone. Habit to these painkillers is non as common as one time thought. Many people who genuinely need these drugs for pain control typically do not become addicted. Nevertheless, narcotic use should be limited to patients thought to have a short life span (such as people with concluding cancer) or patients whose hurting is only expected to final for a short time (such equally people recovering from surgery). In Baronial 2004, the Drug Enforcement Assistants (DEA) issued new guidelines to help physicians prescribe narcotics appropriately without fearfulness of beingness arrested for prescribing the drugs beyond the scope of their medical do. DEA is trying to piece of work with physicians to ensure that those who need to drugs receive them but to ensure opioids are not abused.
Anticonvulsants, as well every bit antidepressant drugs, were initially developed to treat seizures and depression, respectively. However, information technology was discovered that these drugs too have pain-killing applications. Furthermore, since in cases of chronic or extreme hurting, information technology is non unusual for an individual to suffer some degree of depression; antidepressants may serve a dual role. Commonly prescribed anticonvulsants for pain include phenytoin, carbamazepine, and clonazepam. Tricyclic antidepressants include doxepin, amitriptyline, and imipramine.
Intractable (unrelenting) pain may be treated by injections direct into or near the nerve that is transmitting the hurting bespeak. These root blocks may also exist useful in determining the site of pain generation. As the underlying mechanisms of aberrant pain are uncovered, other pain medications are existence developed.
Drugs are not always effective in controlling pain. Surgical methods are used as a terminal resort if drugs and local anesthetics fail. The least subversive surgical procedure involves implanting a device that emits electrical signals. These signals disrupt the nerve and prevent it from transmitting the pain message. However, this method may not completely control pain and is not used frequently. Other surgical techniques involve destroying or severing the nerve, but the utilise of this technique is limited past side effects, including unpleasant numbness.
Culling treatment
Both physical and psychological aspects of pain tin exist dealt with through alternative treatment. Some of the near pop treatment options include acupressure and acupuncture, massage, chiropractic, and relaxation techniques such as yoga, hypnosis, and meditation. Herbal therapies are gaining increased recognition as viable options; for case, capsaicin, the component that makes cayenne peppers spicy, is used in ointments to relieve the joint hurting associated with arthritis. Contrast hydrotherapy can also be very beneficial for pain relief.
Lifestyles can exist changed to incorporate a healthier diet and regular exercise. Regular exercise, bated from relieving stress, has been shown to increase endorphins, painkillers naturally produced in the body.
Prognosis
Successful pain treatment is highly dependent on successful resolution of the pain's cause. Acute pain will stop when an injury heals or when an underlying problem is treated successfully. Chronic pain and abnormal pain are more than difficult to care for, and information technology may take longer to find a successful resolution. Some hurting is intractable and volition crave extreme measures for relief.
Prevention
Pain is generally preventable only to the degree that the cause of the pain is preventable. For case, improved surgical procedures, such as those done through a thin tube called a laparascope, minimize mail service-operative pain. Anesthesia techniques for surgeries also continuously improve. Some disease and injuries are often unavoidable. However, pain from some surgeries and other medical procedures and standing pain are preventable through drug treatments and alternative therapies.
Resources
Periodicals
"Advances in Hurting Management, New Focus Greatly Easing Postoperative Care." Medical Devices & Surgical Applied science Calendar week September 26, 2004: 260.
Finn, Robert. "More than Half of Patients With Major Low Have Chronic Pain." Family Practice News October 15, 2004: 38.
"New Guidelines Set for Better Hurting Treatment." Medical Letter on the CDC & FDA September 5, 2004: 95.
Organizations
American Chronic Hurting Association. P.O. Box 850, Rocklin, CA 95677-0850. (916) 632-0922. 〈http://members.tripod.com/∼widdy/ACPA.html〉.
American Hurting Guild. 4700 Westward. Lake Ave., Glenview, IL 60025. (847) 375-4715. http://www.ampainsoc.org.
Key terms
Acute pain — Pain in response to injury or another stimulus that resolves when the injury heals or the stimulus is removed.
Chronic hurting — Pain that lasts beyond the term of an injury or painful stimulus. Can too refer to cancer pain, pain from a chronic or degenerative disease, and pain from an unidentified crusade.
Neurotransmitters — Chemicals inside the nervous system that transmit data from or betwixt nerve cells.
Nociceptor — A neuron that is capable of sensing pain.
Referred hurting — Pain felt at a site unlike from the location of the injured or diseased part of the trunk. Referred hurting is due to the fact that nerve signals from several areas of the body may "feed" the same nerve pathway leading to the spinal string and brain.
Stimulus — A factor capable of eliciting a response in a nerve.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
pain
[pān]a feeling of distress, suffering, or agony, caused by stimulation of specialized nerve endings. Its purpose is chiefly protective; information technology acts as a alarm that tissues are being damaged and induces the sufferer to remove or withdraw from the source. The N American Nursing Diagnosis Association has accepted hurting as a nursing diagnosis, defining it as a state in which an individual experiences and reports severe discomfort or an uncomfortable sensation; the reporting of pain may exist either by direct verbal communication or by encoded descriptors.
Pain Receptors and Stimuli. All receptors for pain stimuli are free nerve endings of groups of myelinated or unmyelinated neural fibers abundantly distributed in the superficial layers of the pare and in certain deeper tissues such every bit the periosteum, surfaces of the joints, arterial walls, and the falx and tentorium of the cranial crenel. The distribution of hurting receptors in the gastrointestinal mucosa plainly is similar to that in the skin; thus, the mucosa is quite sensitive to irritation and other painful stimuli. Although the parenchyma of the liver and the alveoli of the lungs are almost entirely insensitive to hurting, the liver and bile ducts are extremely sensitive, as are the bronchi and parietal pleura.
Some pain receptors are selective in their response to stimuli, merely most are sensitive to more than 1 of the following types of excitation: (1) mechanical stress of trauma; (2) extremes of heat and common cold; and (three) chemical substances, such as histamine, potassium ions, acids, prostaglandins, bradykinin, and acetylcholine. Hurting receptors, unlike other sensory receptors in the body, exercise not accommodate or become less sensitive to repeated stimulation. Under sure atmospheric condition the receptors go more sensitive over a period of time. This accounts for the fact that as long every bit a traumatic stimulus persists the person volition proceed to exist enlightened that damage to the tissues is occurring.
The body is able to recognize tissue damage because when cells are destroyed they release the chemical substances previously mentioned. These substances tin can stimulate pain receptors or cause direct impairment to the nerve endings themselves. A lack of oxygen supply to the tissues can likewise produce hurting by causing the release of chemicals from ischemic tissue. Muscle spasm is another cause of pain, probably because it has the indirect effect of causing ischemia and stimulation of chemosensitive pain receptors.
Transmission and Recognition of Hurting. When superficial pain receptors are excited the impulses are transmitted from these surface receptors to synapses in the gray matter (substantia gelatinosa) of the dorsal horns of the spinal cord. They then travel up forth the sensory pathways to the thalamus, which is the main sensory relay station of the brain. The dorsomedial nucleus of the thalamus projects to the prefrontal cortex of the encephalon. The witting perception of pain probably takes place in the thalamus and lower centers; interpretation of the quality of hurting is probably the role of the cerebral cortex.
The perception of hurting by an individual is highly circuitous and individualized, and is subject to a multifariousness of external and internal influences. The cerebral cortex is concerned with the appreciation of pain and its quality, location, type, and intensity; thus, an intact sensory cortex is essential to the perception of hurting. In addition to neural influences that transmit and attune sensory input, the perception of pain is afflicted past psychological and cultural responses to pain-related stimuli. A person can be unaware of hurting at the fourth dimension of an acute injury or other very stressful state of affairs, when in a land of depression, or when experiencing an emotional crisis. Cultural influences also precondition the perception of and response to painful stimuli. The reaction to similar circumstances can range from consummate stoicism to histrionic behavior.
Pain Control. At that place are several theories related to the physiologic control of hurting but none has been completely verified. One of the best known is that of Mellzak and Wall, the gate control theory, which proposed that hurting impulses were mediated in the substantia gelatinosa of the spinal string with the dorsal horns interim equally "gates" that controlled entry of pain signals into the central pain pathways. Also, pain signals would compete with tactile signals with the ii constantly balanced confronting each other.
Since this theory was first proposed, researchers take shown that the neuronal circuitry it hypothesizes is not precisely correct. Yet, there are internal systems that are now known to occur naturally in the torso for controlling and mediating pain. I such system, the opioid arrangement, involves the production of morphinelike substances called enkephalins and endorphins. Both are naturally occurring analgesics plant in various parts of the brain and spinal cord that are concerned with pain perception and the transmission of pain signals. Signals arising from stimulation of neurons in the grey matter of the brain stem travel downward to the dorsal horns of the spinal cord where incoming pain impulses from the periphery stop. The descending signals cake or significantly reduce the transmission of hurting signals upward along the spinal cord to the brain where hurting is perceived by releasing these substances.
In addition to the encephalon'due south opioid organisation for controlling the transmission of pain impulses along the spinal cord, at that place is another mechanism for the control of pain. The stimulation of large sensory fibers extending from the tactile receptors in the pare can suppress the manual of pain signals from thinner nerve fibers. It is every bit if the nerve pathways to the brain can adjust only one blazon of bespeak at a time, and when two kinds of impulses simultaneously go far at the dorsal horns, the tactile sensation takes precedence over the sensation of hurting.
The discovery of endorphins and the inhibition of pain transmission by tactile signals has provided a scientific explanation for the effectiveness of such techniques every bit relaxation, massage, application of liniments, and acupuncture in the control of pain and discomfort.
Assessment of Pain. Pain is a subjective miracle that is present when the person who is experiencing it says it is. The person reporting personal discomfort or pain is the well-nigh reliable source of information about its location, quality, intensity, onset, precipitating or aggravating factors, and measures that bring relief.
Objective signs of hurting tin assist verify what a patient says nearly pain, merely such data are not used to evidence or disprove whether it is present. Physiologic signs of moderate and superficial pain are responses of the sympathetic nervous system. They include rapid, shallow, or guarded respiratory movements, pallor, diaphoresis, increased pulse rate, elevated blood pressure, dilated pupils, and tenseness of the skeletal muscles. Hurting that is severe or located deep in body cavities acts every bit a stimulant to parasympathetic neurons and is evidenced by a drop in blood pressure level, slowing of pulse, pallor, nausea and vomiting, weakness, and sometimes a loss of consciousness.
Behavioral signs of pain include crying, moaning, tossing about in bed, pacing the floor, lying quietly merely tensely in one position, drawing the knees upwards toward the belly, rubbing the painful part, and a pinched facial expression or grimacing. The person in pain also may have difficulty concentrating and remembering and may be totally self-centered and preoccupied with the pain.
Psychosocial aspects of tolerance for hurting and reactions to it are less easily identifiable and more than complex than physiologic responses. An individual's reaction to pain is subject to a variety of psychologic and cultural influences. These include previous experience with pain, training in regard to how ane should answer to pain and discomfort, land of health, and the presence of fatigue or physical weakness. One'south degree of attending to and distraction from painful stimuli can also impact one's perception of the intensity of pain. A thorough assessment of hurting takes into consideration all of these psychosocial factors.
Direction of Pain. Among the measures employed to provide relief from pain, administration of analgesic drugs is probably the 1 that is most often misunderstood and abused. When an analgesic drug has been ordered "as needed," the patient should know that the drug is truly bachelor when needed and that information technology volition be given promptly when asked for. If the patient is forced to wait until someone else decides when an analgesic is needed, the patient may become angry, resentful, and tense, thus diminishing or completely negating the desired effect of the drug. Studies have shown that when analgesics are left at the bedside of terminally ill cancer patients to be taken at their discretion, fewer doses are taken than when they must rely on someone else to make the drug bachelor. Habituation and addiction to analgesics probably result as much from non using other measures along with analgesics for pain control every bit from giving prescribed analgesics when they are ordered. Patient-controlled analgesia has been used safely and effectively.
When analgesics are not appropriate or sufficient or when there is a real danger of addiction, there are noninvasive techniques that tin can exist used as alternatives or adjuncts to analgesic therapy. The option of a particular technique for the management of pain depends on the cause of the pain, its intensity and elapsing, whether information technology is acute or chronic, and whether the patient perceives the technique equally effective.
Distraction techniques provide a kind of sensory shielding to make the person less aware of discomfort. Lark tin be effective in the relief of brief periods of acute pain, such as that associated with minor surgical procedures under local anesthesia, wound débridement, and venipuncture.
Massage and gentle pressure level activate the thick-cobweb impulses and produce a preponderance of tactile signals to compete with pain signals. It is interesting that stimulation of the big sensory fibers leading from superficial sensory receptors in the skin can relieve pain at a site distant from the area being rubbed or otherwise stimulated. Since ischemia and muscle spasm tin can both produce discomfort, massage to ameliorate circulation and frequent repositioning of the body and limbs to avoid circulatory stasis and promote musculus relaxation can exist effective in the prevention and direction of pain. Transcutaneous electrical nerve stimulation (TENS) units raise the production of endorphins and enkephalins and can also relieve pain.
Specific relaxation techniques can aid relieve physical and mental tension and stress and reduce pain. They have been especially constructive in mitigating discomfort during labor and delivery but tin can exist used in a variety of situations. Learning proper relaxation techniques is not easy for some people, simply one time these techniques have been mastered they can be of nifty benefit in the direction of chronic ongoing pain. The intensity of pain too can be reduced by stimulating the peel through applications of either oestrus or cold, menthol ointments, and liniments. Contralateral stimulation involves stimulating the skin in an area on the side opposite a painful region. Stimulation tin can exist done by rubbing, massaging, or applying oestrus or common cold.
Since pain is a symptom and therefore of value in diagnosis, information technology is important to keep accurate records of the observations of the patient having pain. These observations should include the following: the nature of the pain, that is, whether information technology is described by the patient as being abrupt, deadening, burning, aching, etc.; the location of the pain, if the patient is able to decide this; the fourth dimension of onset and the elapsing, and whether or non certain nursing measures and drugs are successful in obtaining relief; and the relation to other circumstances, such every bit the position of the patient, occurrence before or after eating, and stimuli in the surround such equally rut or cold that may trigger the onset of pain.
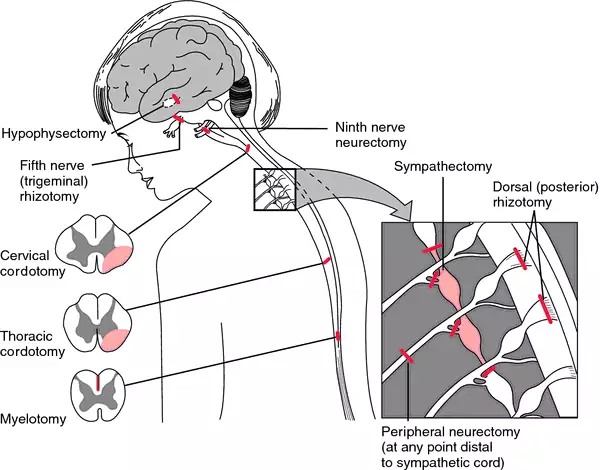
Surgical procedures designed to alleviate pain. From Ignatavicius et al., 1999.
acute pain
ane. one of the three categories of hurting established by the International Association for the Study of Pain, denoting hurting that is caused past occurrences such as traumatic injury, surgical procedures, or medical disorders; clinical symptoms ofttimes include increased middle rate, blood pressure, and respiratory charge per unit, shallow respiration, agitation or restlessness, facial grimaces, or splinting.
two. a nursing diagnosis accepted by the N American Nursing Diagnosis Association, divers every bit an unpleasant sensory and emotional experience arising from actual or potential tissue impairment or described in terms of such harm, with sudden or slow onset of whatever intensity from mild to astringent with an anticipated or anticipated terminate and a duration of less than 6 months.
bearing-down pain hurting accompanying uterine contractions during the 2d phase of labor.
cancer hurting one of the three categories of hurting established past the International Association for the Study of Pain, cogent pain associated with malignancies and perceived past the individual patient; there are various scales ranking information technology from 0 to 10 according to level of severity.
chronic pain
1. one of the three categories of hurting established by the International Clan for the Study of Pain, denoting hurting that is persistent, often lasting more than than six months; clinical symptoms may exist the aforementioned as for acute pain, or at that place may be no symptoms evident. The North American Nursing Diagnosis Association has accepted chronic pain equally a nursing diagnosis.
2. a nursing diagnosis accustomed past the North American Nursing Diagnosis Association, defined as an unpleasant sensory and emotional experience arising from bodily or potential tissue harm or described in terms of such damage, with sudden or boring onset of any intensity from mild to astringent, without an anticipated or predictable end, and with a duration of greater than 6 months.
pain disorder a somatoform disorder characterized by a master complaint of severe chronic hurting that causes substantial distress or impairment in functioning; the hurting is neither feigned nor intentionally produced, and psychological factors appear to play a major role in its onset, severity, exacerbation, or maintenance. The pain is related to psychological conflicts and is made worse by ecology stress; it enables the patient to avoid an unpleasant activity or to obtain support and sympathy. Patients may visit many health intendance providers searching for relief and may consume excessive amounts of analgesics without whatever effect. They are difficult to treat because they strongly resist the idea that their symptoms have a psychological origin.
simulated p'south ineffective pains during pregnancy that resemble labor pains, not accompanied by cervical dilatation; see also braxton-hicks contractions. Called also faux labor.
growing p'southward whatever of diverse types of recurrent limb pains resembling those of rheumatoid conditions, seen in early youth and formerly idea to exist acquired by the growing process.
hunger pain pain coming on at the fourth dimension for feeling hunger for a meal; a symptom of gastric disorder.
intermenstrual pain pain accompanying ovulation, occurring during the period betwixt the flow, ordinarily about midway.
labor p's the rhythmic pains of increasing severity and frequency due to wrinkle of the uterus at childbirth; see also labor.
lancinating pain abrupt darting pain.
phantom hurting pain felt as if information technology were arising in an absent or amputated limb or organ; see too amputation.
psychogenic pain symptoms of physical pain having psychological origin; run into pain disorder.
referred pain hurting in a part other than that in which the crusade that produced it is situated. Referred pain usually originates in one of the visceral organs but is felt in the pare or sometimes in some other area deep inside the body. Referred pain probably occurs because pain signals from the viscera travel along the same neural pathways used by pain signals from the skin. The person perceives the pain but interprets it equally having originated in the peel rather than in a deep-seated visceral organ.
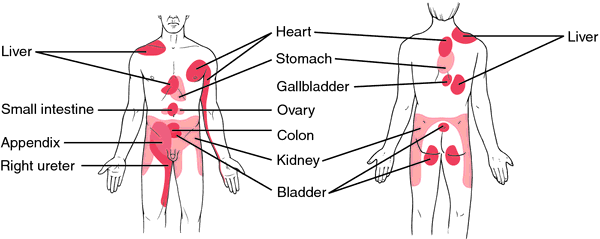
Area of referred pain, anterior and posterior views.
rest pain a continuous unrelenting pain due to ischemia of the lower leg, kickoff with or being aggravated by acme and being relieved by sitting with legs in a dependent position or by standing.
root pain pain caused past illness of the sensory nerve roots and occurring in the cutaneous areas supplied by the affected roots.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Wellness, Seventh Edition. © 2003 by Saunders, an banner of Elsevier, Inc. All rights reserved.
pain
(pān),i. A variably unpleasant sensation associated with actual or potential tissue damage and mediated by specific nerve fibers to the brain where its conscious appreciation may exist modified by various factors.
2. Term used to denote a painful uterine contraction occurring in childbirth.
[50. poena, a fine, a punishment]
pain
algophobia.
Farlex Partner Medical Dictionary © Farlex 2012
pain
(pān)n.
i. An unpleasant feeling occurring as a result of injury or disease, usually localized in some part of the body.
2. Mental or emotional suffering; distress.
iii. One of the uterine contractions occurring in childbirth.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published past Houghton Mifflin Company. All rights reserved.
pain
Neurology 'An unpleasant sensory and emotional experience associated with bodily or potential tissue damage or described in terms of such damage'-per Intl Assn for Written report of Hurting; a awareness of discomfort, distress, or agony, due to stimulation of specialized nerve endings; a sensation of marked discomfort, either precipitous and well-localized–conducted along A-delta fibers or dull and diffuse–conducted forth C nerve fibers. See Astute pain, Acute depression back pain, Ankle pain, Dorsum pain, Breakthrough pain, Brief Pain Inventory, Key stroke pain, Chest pain, Chest wall pain, Chronic pain, Discogenic pain, Elbow pain, Gait control theory, Growing pain, Intractable pain, Genu hurting, Lightning pain, Low back hurting, Noncardiac chest pain, Patient controlled analgesia, Phantom limb hurting, Substantial pain, Suprapubic pain.McGraw-Hill Curtailed Lexicon of Modern Medicine. © 2002 by The McGraw-Loma Companies, Inc.
pain
(pān)An unpleasant sensation associated with bodily or potential tissue damage, and mediated by specific nerve fibers to the brain, where its witting appreciation may exist modified by various factors.
[50. poena, a fine, a penalty]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
hurting
(pan) [Fr. peine, fr L. poena, a fine, a punishment, punishment]As divers past the International Clan for the Written report of Pain, an unpleasant sensory and emotional experience arising from bodily or potential tissue impairment or described in terms of such damage. Pain includes not but the perception of an uncomfortable stimulus but also the response to that perception. Well-nigh half of those who seek medical help exercise so considering of the primary complaint of pain. Acute hurting occurs with an injury or affliction; is frequently accompanied by anxiety, diaphoresis, nausea, and vital sign changes such as tachycardia or hypertension; and should end subsequently the baneful stimulus is removed or any organ damage heals. Chronic or persistent hurting is discomfort that lasts beyond the normal healing menstruation. Pain may arise in nearly any organ system and may take different characteristics in each. Musculoskeletal pain often is exacerbated by motion and may be accompanied by joint swelling or musculus spasm. Myofascial pain is marked by trigger-point tenderness. Visceral pain often is diffuse or vaguely localized, whereas hurting from the lining of body cavities often is localized precisely, very intense, and exquisitely sensitive to palpation or motility. Neuropathic (nerve) pain usually stings or burns, or may be described as numbness, tingling, or shooting sensations. Colicky pain fluctuates in intensity from severe to mild, and ordinarily occurs in waves. Referred hurting results when an injury or disease occurs in one body part but is felt in another.
Several factors influence the experience of pain. Among these are the nature of the injury or illness causing the symptom, the physical and emotional wellness of the patient, the acuity or chronicity of the symptom, the social milieu and/or cultural upbringing of the patient, neurochemistry, memory, personality, and other features. See: table
Symptoms
Many clinicians utilize the mnemonic "COLDER" to assistance the diagnosis of painful diseases. They will ask the patient to describe the Character, Onset, 50ocation, and Duration of their painful symptoms, as well every bit the features that Exacerbate or Relieve it. For instance: The hurting of pleurisy typically is abrupt in grapheme, acute in onset, located along the chest wall, and long-lasting; it is worsened by deep breathing or coughing and relieved by analgesics or holding still. By dissimilarity, the pain of myocardial ischemia usually is dull or heavy, gradual in onset, and located substernally. It may exist worsened by activity (just not by taking a jiff or coughing) and relieved by nitroglycerin.
In 2000, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) issued hurting-management standards, in 2001 began surveying for compliance, and in 2004 added patient-safety goals, thus nearly U.S. health care facilities have devised policies and procedures that crave pain-intensity rating as a routine part of care (the fifth vital sign). Pain intensity usually is assessed on a numerical scale, in which 0 = no pain, 1 to iii = mild pain, 4 to 6 = moderate pain, and seven to 10 = severe hurting. However, obtaining a numerical rating of pain intensity is possible only if the patient is able to provide this study of the pain being experienced, which infants, children, the critically ill, and cognitively dumb normally are unable to do. The Wong' Bakery FACES calibration, developed for pediatric use, has been used successfully in other patient populations. It uses visual representations of smiles or grimaces to draw the level of pain a patient feels.
Patient care
Health intendance professionals must be aware that pain in non-verbal patient tin easily exist overlooked and must brand a witting try to ensure that pain in these patients is assessed and treated. Observing subtle behaviors and being sensitive to contextual clues are 2 pain methods used by health care professionals to effort to make up one's mind when nonverbal patients are in pain. When this judgment is fabricated, a trial of pain-relieving medication may exist used. The responses of the patient and any complications of treatment should exist carefully observed and appropriate changes fabricated in dosing or the type of analgesic drug as indicated.
Because pain is a subjective and intensely personal problem, sympathetic care is an important office of its relief. In addition to administering analgesic drugs, wellness intendance professionals should use a wide range of techniques to help alleviate pain, including local application of common cold and estrus, tactile stimulation, relaxation techniques, diversion, and active listening, amidst others.
acute pain
Pain that typically is produced by sudden injury (e.g., fracture) or illness (eastward.thou., acute infection) and is accompanied by concrete signs such every bit increased heart rate, elevated blood pressure, pupillary dilation, sweating, or hyperventilation. Acute pain is typically abrupt in character. It is relayed to the central nervous arrangement rapidly past A delta nerve fibers. [And so, at the terminate of this entry please add the SYN:] fast pain Depending on the severity of the underlying stimulus, acute pain may be managed with acetaminophen or anti-inflammatory drugs, immobilization and summit of the injured body part, or the topical application of heat or ice. Severe acute pain, such as that of broken ribs or of an ischemic function, may crave narcotics, ofttimes with adjunctive agents like hydroxyzine for relief, or antiemetics. Acute pain should be managed aggressively. Synonym: fast pain
adnexal pain
Discomfort arising from the fallopian tubes and ovaries; usually due to inflammation, infection, or ectopic pregnancy.
back pain
Pain felt in or along the spine or musculature of the posterior thorax. It is unremarkably characterized by dull, continuous pain and tenderness in the muscles or their attachments in the lower lumbar, lumbosacral, or sacroiliac regions. Back pain is oftentimes referred to the leg or legs, following the distribution of the sciatic nerve.
Etiology
Mutual causes of dorsum pain include hurting caused past muscular or tendon strain, herniated intervertebral disk, lumbar spinal stenosis, or spondylolisthesis. Patients with a history of cancer may have back pain acquired by metastatic tumors to the vertebrae and should exist evaluated to be sure that impairment to the spinal string is not imminent. Patients with dorsum hurting and fever (esp. those with a history of injection drug utilise, tuberculosis, or contempo back surgery) should exist evaluated for epidural abscess or osteomyelitis.
Treatment
Depending on the underlying crusade of the dorsum pain, treatment may include drugs, rest, massage, physical therapy, chiropractic, stretching exercises, injection therapy, and surgery, among others. Most nonmalignant causes of back pain improve with a few days of remainder, analgesics, and antiinflammatory drugs, followed by ii to 4 weeks of anti-inflammatory treatment, appropriate muscle strengthening, and patience. Pain caused by an osteoporotic fracture may prove more debilitating and longer-lasting. Back pain produced by a spinal metastasis can improve with corticosteroids, radiation therapy, intravenous bisphosphonates, and/or surgical decompression. Patients with a spinal epidural abscess will need surgical drainage of the infection and antibiotics.
Patient intendance
Prolonged bedrest is inadvisable in most patients with back pain. The handling regimen is explained, implemented, and reinforced. Factors that precipitate symptoms are identified and preventive deportment are discussed.
bearing-downwardly pains
Rectal pressure and discomfort occurring during the second stage of labor, related to fetal descent and the woman'due south straining efforts to expel the fetus.
tedious pain
Piercing, used to describe pain felt deep within the body.
quantum pain
Transient episodes of pain that occur in patients with chronic pain that has been previously reduced to tolerable levels. Breakthrough hurting disrupts the well-beingness of cancer or hospice patients who have been prescribed regular doses of narcotic analgesics. The painful episodes may occur as a previous dose of hurting-relieving medication wears off ("stop-of-dose pain"), or after unusual or unanticipated body movements ("incident hurting").
Brodie pain
Pain caused most a joint affected with neuralgia when the peel is folded near it.
burning hurting
Pain experienced in heat burns, superficial peel lesions, herpes zoster, and circumscribed neuralgias.
causalgic pain
Causalgia.central pain
Pain due to a lesion in the central nervous system.
chest pain
Discomfort felt in the upper abdomen, thorax, neck, or shoulders. Chest pain is i of the most common potentially serious complaints offered past patients in emergency departments, hospitals, outpatient settings, and physicians' offices. A broad array of diseases and conditions may cause information technology, including (but non limited to) angina pectoris or myocardial infarction; feet and hyperventilation; aortic dissection; costochondritis or injured ribs; cough, pneumonia, pleurisy, pneumothorax, or pulmonary emboli; esophageal diseases, such as reflux or esophagitis; gastritis, duodenitis, or peptic ulcer; and stones in the biliary tree.
chronic idiopathic pelvic pain
Abbreviation: CIPPUnexplained pelvic pain in a adult female that has lasted 6 months or longer. A complete medical, social, and sexual history must be obtained. In an experimental study, women with this illness reported more sexual partners, significantly more spontaneous abortions, and previous nongynecological surgery. These women were more likely to accept experienced previous significant psychosexual trauma.
Handling
The pain associated with CIPP should exist treated symptomatically and sympathetically. The participation of pain management specialists, complementary medical providers, and the primary wellness care provider should be integrated. Realistic goals (e.chiliad., the reduction of pain rather than its elimination) should be prepare. Medroxyprogesterone acetate, oral contraceptives, presacral neurectomy, hypnosis, and hysterectomy accept been tried with varying degrees of success.
chronic pain
i. Long-lasting discomfort, with episodic exacerbations, that may be felt in the back, one or more joints, the pelvis, or other parts of the trunk.
2. Pain that lasts more than three–vi months.
iii. Pain that lasts more than than a month longer than the usual or expected course of an disease.
4. Pain that returns periodically every few weeks or months for many years. Chronic pain is often described past sufferers as existence debilitating, intolerable, disabling, or alienating and may occur without an easily identifiable cause. Studies accept shown a loftier correlation between chronic pain and low or dysphoria, but information technology is unclear whether the psychological aspects of chronic hurting precede or develop as a result of a person'due south subjective suffering. Chronic pain is the leading crusade of inability in the U.s.acute pain;
Patient care
The management of chronic, nonmalignant pain is often difficult and may be frustrating for both sufferer and caregiver. The best results are usually obtained through multimodal therapy that combines sympathetic guidance that encourages patients to recover functional abilities, by combinations of drugs (eastward.g., nonsteroidal anti-inflammatories, narcotic analgesics, and/or antidepressants), physical therapy and regular exercise, occupational therapy, physiatry, psychological or social counseling, and alternative medical therapies (e.g., acupuncture, massage, or relaxation techniques). Placebos, although rarely employed clinically, effectively treat chronic pain in most a third of all patients. Surgery and other invasive strategies are occasionally employed, with variable effectiveness.
cramplike pain
Cramp.dental pain
Pain in the oral area, which, in full general, may exist of two origins. Soft tissue hurting may exist astute or chronic, and a called-for pain is due to surface lesions and usually can exist discretely localized; pulpal pain or tooth pain varies according to whether it is acute or chronic, but information technology is often difficult to localize.
dilating hurting
Discomfort accompanying rhythmic uterine contractions during the first stage of labor.
diskogenic hurting
Depression back pain resulting from degeneration of an intervertebral deejay. Discogenic pain differs from neuropathic hurting in that it does not radiate into the extremities or torso.
tedious pain
A mild discomfort, oftentimes hard to draw, that may be associated with some musculoskeletal injuries or some diseases of the visceral organs.
eccentric hurting
Hurting occurring in peripheral structures owing to a lesion involving the posterior roots of the spinal nerves.
epigastric pain
Hurting located between the xiphoid process and the omphalos. It may suggest a problem in ane of many different organs, including the stomach, pancreas, gallbladder, small or large bowel, pleura, or centre.
Synonym: gastralgic hurting Encounter: cardialgiaexpulsive pains
Discomfort during the 2d stage of labor, associated with bearing-downward efforts to expel the fetus. Women may feel a like hurting during commitment of the placenta.
false pain
Intestinal discomfort associated with Braxton Hicks contractions, which occur during the last trimester of pregnancy. Characteristically, the woman complains of irregular, lower abdominal pains, which are relieved by walking. Vaginal examination shows no change in cervical effacement or dilation.
Encounter: Braxton Hicks contractionsfast hurting
Acute pain.fulgurant pain
Lightning pain.gallbladder pain
Biliary colic.gas hurting
Pain in the intestines acquired past an accumulation of gas therein.
gastralgic pain
Epigastric pain.girdle hurting
Zonesthesia.growing pains
An imprecise term indicating ill-defined pain, normally in the shin or other areas of the legs, typically occurring later bedtime in children age 5 to 12. At that place is no evidence that the pain is related to rapid growth or to emotional problems. If these symptoms occur during the daytime, are accompanied by other symptoms, or get progressively more astringent, evaluation for infection, cancer, and other diseases of muscle and bone should be undertaken. In the bulk of cases, this evaluation is not necessary.
Handling
The child should be reassured and given acetaminophen or ibuprofen; heat and massage tin can be applied locally. Children with growing pains benefit from concern and reassurance from their parents and health intendance providers.
heterotopic pain
Referred pain.homotopic hurting
Hurting felt at the indicate of injury.
hunger hurting
Pain in the epigastrum that occurs before meals.
incident pain
Pain due to a sudden, forceful, unanticipated, or unusual trunk motility or posture.
inflammatory hurting
Pain in the presence of inflammation that is increased past pressure.
intermenstrual pain
Episodic, localized pelvic discomfort that occurs between menstrual periods, perhaps accompanying ovulation.
Synonym: midpain Run across: mittelschmerzintractable pain
Chronic pain that is hard or impossible to manage with standard interventions. Common causes include metastatic cancer, chronic pancreatitis, radiculopathy, spinal string transection, or peripheral neuropathy. Intractable pain may also accompany somatoform disorders, depression, fibromyalgia, irritable bowel syndrome, and opiate dependence. Diverse combinations of the following management strategies are oft used to care for intractable hurting: antidepressant medications, counseling, deep brain stimulation, injected anesthetics, narcotic analgesics, neurological surgery, and pain clinic consultations.
labor pains
Uncomfortable, intermittent, rhythmic, girdling sensations associated with uterine contractions during childbearing. The frequency, duration, and intensity of the events increase, climaxing with the delivery of the fetus.
lancinating hurting
Astute pain.lightning pain
A sudden brief pain that may be repetitive, unremarkably in the legs but may be at any location. It is associated with tabes dorsalis and other neurological disorders. Synonym: fulgurant pain
lingual pain
Pain in the tongue that may be due to local lesions, glossitis, fissures, or pernicious anemia. Synonym: tongue pain
lung pain
Sharp pain in the region of the lungs.
menstrual pain
Dysmenorrhea.mental pain
Psychogenic pain.middle pain
Intermenstrual pain.mobile pain
Pain that moves from one area to another.
motion pain
Kinesalgia.neuropathic hurting
Pain that originates in peripheral fretfulness or the central nervous system rather than in other damaged organs or tissues. A hallmark of neuropathic pain is its localization to specific dermatomes or nerve distributions. Some examples of neuropathic pain are the pain of shingles (herpes zoster), diabetic neuropathy, radiculopathy, and phantom limb pain.
Treatment
Drugs like gabapentin or pregabalin provide effective relief of neuropathic pain for some patients. Other treatments include (but are not express to) regional nervus blocks, selective serotonin and norepinephrine reuptake inhibitors, psychological counseling, acupuncture, transcutaneous electrical nerve stimulation, and physical therapy.
night pain
Pain that awakens the patient at night or interferes with sleep; may exist due to infection, inflammation, neurovascular compromise, or severe structural damage.
noise pain
Odynacusis.objective pain
Pain induced by some external or internal irritant, by inflammation, or by injury to nerves, organs, or other tissues that interferes with the function, nutrition, or circulation of the affected part. It is usually traceable to a definite pathologic process.
paresthesic hurting
A stinging or tingling sensation manifested in central and peripheral nervus lesions.
See: paresthesiaperiodontal pain
A discrete, well-localized pain caused by inflammation of tissues surrounding a molar. This may be contrasted with the throbbing, nonlocalized hurting typical of a toothache or pulpal hurting.
phantom limb pain
The sensation of pain felt in the nervus distribution of a body part that has been amputated. Phantom pain can pb to difficulties in prosthetic training. Synonym: phantom sensation
Patient care
Phantom limb pain or nonpainful sensations are reported by most amputees. A multimodal or combination arroyo to management is appropriate. Drugs used to treat neuropathic pain may be helpful, including some anticonvulsant drugs, tricyclic antidepressants, selective serotonin inhibitors, and muscle relaxants. Nervus blockade and/or transcutaneous electrical stimulation may also be helpful. Wellness care professionals should encourage amputees to move the affected extremity, seek counseling or group therapy, appoint in concrete and occupational therapy, and utilise lark techniques.
postprandial pain
Abdominal pain after eating.
precordial hurting
Pain felt in the heart of the chest (eastward.g., beneath the sternum) or in the left side of the chest.
premonitory pain
Ineffective contractions of the uterus before the first of truthful labor.
See: imitation hurtingpseudomyelic pain
The false awareness of move in a paralyzed limb or of no movement in a moving limb; not a true hurting.
psychogenic hurting
Pain having mental, equally opposed to organic, origin.
radicular pain
Pain that radiates abroad from the spinal cavalcade through an extremity or the torso resulting from the compression or irritation of a spinal nerve root or large paraspinal nervus. It may exist accompanied by numbness or tingling.
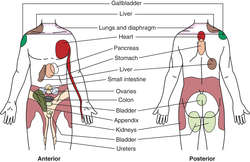
![]()
SITES OF REFERRED Pain
referred pain
Pain that arises in 1 torso part or location merely is perceived in another. For example, hurting caused past inflammation of the diaphragm often is felt in the shoulder; hurting caused by myocardial ischemia may be referred to the neck or jaw; and pain caused by appendicitis may commencement be felt almost the umbilicus rather than in the correct lower quadrant, where the appendix lies. See: tabular array
Synonym: heterotopic hurting; sympathetic pain Come across: analogyremittent pain
Pain with temporary abatements in severity; characteristic of neuralgia and colic.
rest pain
Pain due to ischemia that comes on when sitting or lying.
root pain
Cutaneous pain caused by disease of the sensory nerve roots.
shooting hurting
Pain that seems to travel similar lightning from one place to another.
dull pain
Pain that is perceived a second or more than afterwards a stimulus. It is transmitted to the key nervous system by C (nervus) fibers, which are not myelinated, and therefore conduct sensations more slowly than A delta fibers. Irksome pain lasts longer than sudden pain. It is usually perceived by patients as called-for, cramping, dull, itchy, or warm.
standards for pain relief
Standards for the Relief of Acute Pain and Cancer Hurting developed by the American Hurting Gild. These are summarized every bit follows:
1. In order to increase the clinician's responsiveness to complaints of pain, it is now considered by some health care professionals to be the fifth vital sign.two. Astute pain and cancer pain are recognized and finer treated. Essential to this procedure is the development of a clinically useful and easy-to-utilize scale for rating pain and its relief. Patients volition be evaluated according to the scales and the results recorded as often as needed.iii. Data virtually analgesics is readily available. This includes information concerning the effectiveness of various agents in controlling pain and the availability of equianalgesic charts wherever drugs are used for hurting.4. Patients are informed on admission of the availability of methods of relieving hurting, and that they must communicate the presence and persistence of pain to the health care staff.v. Explicit policies for use of advanced analgesic technologies are defined. These advances include patient-controlled analgesia, epidural analgesia, and regional analgesia. Specific instructions concerning utilize of these techniques must be available for the wellness care staff.6. Adherence to standards is monitored by an interdisciplinary commission. The committee is responsible for overseeing the activities related to implementing and evaluating the effectiveness of these pain standards.
starting hurting
A hurting accompanied by muscular spasm during the early stages of sleep.
subdiaphragmatic hurting
A sharp stitchlike hurting occurring during animate caused, for case, by an abscess or tumor beneath the diaphragm. When the jiff is held, the pain ceases. Pressure level against the lower rib cage eases the hurting.
subjective pain
Psychogenic pain.sympathetic hurting
Referred pain.tenesmic pain
Tenesmus.terebrant pain
A ho-hum or piercing type of hurting.
thalamic pain
See: thalamic syndromethermalgesic hurting
Hurting caused by heat.
thoracic pain
Breast pain.throbbing pain
Hurting constitute in dental caries, headache, and localized inflammation. The pain is often thought to be caused past arterial pulsations.
natural language pain
Lingual pain.tracheal pain
Trachealgia.vascular pain
Pain that throbs or pulses, such as the pain of a migraine headache.
wandering pain
Pain that changes its location repeatedly.
* By mouth unless indicated otherwise.PO—by oral fissure only.SOURCE: Adapted from Isselbacher, K.J., et al.: Harrison'south Principles of Internal Medicine, ed 13. McGraw-Hill, New York, 1994.| Nonopioid Analgesics | |||
|---|---|---|---|
| Generic Name | Dose, mg * | Interval | Comments |
| Acetylsalicylic acid | 325–650 | 4–24 hr | Enteric-coated preparations bachelor |
| Acetaminophen | 650 | four hr | Avoid in liver failure |
| Ibuprofen | 400–800 | iv–8 60 minutes | Available without prescription |
| Indomethacin | 25–75 | 8 hr | Gastrointestinal and kidney side effects common |
| Naproxen | 250–500 | 12 60 minutes | Delayed furnishings may be due to long half-life |
| Ketorolac | 15–lx IM | 4–half-dozen hr | Similar to ibuprofen but more than potent |
| Opioid Analgesics | |||
| Generic Proper name | Parenteral Dose (mg) | PO Dose (mg) | Comments |
| Codeine | 30–threescore every 4 hr | 30–60 every iv hr | Nausea common |
| Hydromorphone | 1–2 every 4 hr | 2–4 every 4 60 minutes | Shorter acting than morphine sulfate |
| Levorphanol | 2 every 6–8 hr | iv every 6 hr | Longer acting than morphine sulfate; absorbed well PO |
| Methadone | 10–100 | 6–24 hr | Delayed sedation due to long half-life |
| Meperidine | 25–100 | 300 every 4 60 minutes | Poorly absorbed PO; normeperidine is a toxic metabolite |
| Morphine | 10 every iv 60 minutes | threescore every four hr | |
| Morphine, sustained release | thirty–90 | 60–180 2 or 3 times daily | |
| Oxycodone | — | v–ten every 4–6 hr | Usually bachelor with acetaminophen or aspirin |
| Organ of Origin | Location Felt |
|---|---|
| Caput | External or centre ear |
| Nose & sinuses | |
| Teeth, gums, natural language | |
| Throat, tonsils | |
| Parotid gland, TMJ joint | |
| Thorax | |
| Diaphragm | Shoulder, upper belly |
| Heart | Upper chest, L shoulder, inside L arm, 50 jaw |
| Abdomen | |
| Stomach & spleen | L upper abdomen |
| Duodenum | Upper abdomen, R shoulder |
| Stomach & spleen | L upper abdomen |
| Stomach & spleen | L upper abdomen |
| Stomach & spleen | L upper abdomen |
| Colon | Lower abdomen |
| Appendix | Periumbilical and R lower belly |
| Pelvis | |
| Appendix | Periumbilical and R lower belly |
Medical Lexicon, © 2009 Farlex and Partners
hurting
An unpleasant or distressing localized sensation caused past stimulation of certain sensory nerve endings chosen nociceptors, or by strong stimulation of other sensory nerves. Nociceptors are stimulated past the chemical action of substances, such every bit prostaglandins, released from local cell damaged by injury or inflammation. Whatever the site of nerve stimulation, hurting is normally experienced in the region of the nerve endings. Referred hurting is pain experienced at a site other than that at which the causal gene is operating. Pain impulses pass to the brain via a serial of control 'gates' coordinating to those in computers and these can be modulated past other nerve impulses. Pain unremarkably serves as a warning of bodily danger and leads to action to finish it. Pain is best treated past discovering and removing the crusade. It is a complex phenomenon with many components-somatic, emotional, cerebral and social. The management of acute, cocky-limiting hurting is not the same every bit long-term pain. The latter requires treatment past a multidisciplinary team in a pain clinic. ANALGESIC drugs can be used to target specific receptors and should non be withheld until pain is astringent simply given repeatedly in expectation of pain. Hurting may be relieved past drugs cocky-administered on an as-required basis; by electrical stimulation of the pare; ACUPUNCTURE; massage; cold sprays; LOCAL ANAESTHETIC injections; or even, in extreme cases and rarely, by permanent nerve destruction by alcohol injection or by surgical severance. From the Latin poena, punishment. Encounter also ENDORPHINS.Collins Dictionary of Medicine © Robert Yard. Youngson 2004, 2005
pain
an unpleasant, conscious sensation produced in the encephalon and stimulated by hurting receptors in, for example, the peel. Pain has a protective function and oft produces a reflex activeness (see REFLEX ARC in response.Collins Dictionary of Biology, 3rd ed. © W. Chiliad. Unhurt, V. A. Saunders, J. P. Margham 2005
pain
(pān)Variably unpleasant sensation associated with tissue impairment and mediated past specific nervus fibers to brain where its conscious appreciation is modified.
[50. poena, a fine, a penalty]
Medical Dictionary for the Dental Professions © Farlex 2012
Patient discussion about pain
Q. Pulling pain in anus. Dear friends, I am 32. I feel a Pulling pain in anus sometimes while i end passing stool and some times when i sit for long fourth dimension. No bleeding then far. Is information technology a symptoms of piles? If so what tin can be done to cure it without going to doctor or functioning. Please assistance me. This hurting makes me to experience that i am very onetime.
A. horsechestnut is supposed to help...here is some info about it:
http://nccam.nih.gov/health/horsechestnut/index.htm#uses
but i wouldn't get my hopes high.
Q. Polio Syndrome pain One of my aunt is taking Neurontin for Mail Polio Syndrome pain in her left leg and arm. she did non realize that she had so much pain and that it was keeping her from doing and so many things. Is Neurontin recomended for this handling and how does it assistance? Will she have issues with Neurontin if she accept it long term? Neurontin is profoundly helping the pain but not the fatique in these limbs. Should it help the fatigue?
A. Neurontin is being given as medication for nerve hurting now likewise...I have 800 mg a day and information technology was started for back pain and it is also being used in some fibro patients I am learning( i besides take fibromyalgia) It didn't cause me a lot of drowsness but amount of medication and medications affect people differently then each person tin be different. But with the fatigue fibromyalgia causes perhaps I just can't tell the divergence b/c before I started information technology I was tried all the fourth dimension and that is not whatever worse. But if your Aunt and yourself feel uncomfortable with this handling I would suggest a second opinion. Good Luck to your Aunt
Q. Why do they recall that the pain is all in my head? Is at that place whatever run a risk which may wrongfully lead doctor to conclude that our symptoms are of a psychological nature? Why exercise they call back that the pain is all in my head?
A. It may happen very rarely and if he is new to his profession. It doesn't hateful that all those are new to their profession does these mistakes. Doctors cannot "run into" and may not understand the sources of your pain or fatigue. However, what they do find is your anxiety and frustration with having to deal with these symptoms around-the-clock, which may wrongfully pb them to conclude that your symptoms are of a psychological nature. Also, the old school of idea regarding pain is that it is produced by tissue injury, and there is no obvious source of tissue injury in patients with fibromyalgia. Regardless, if your doctor does not believe that your symptoms are real, you owe information technology to yourself to notice another doctor who believes in you and will piece of work with you to help reduce your symptoms.
More discussions about hurtingThis content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.
Can Swallowing A Can Tab Kill You,
Source: https://medical-dictionary.thefreedictionary.com/pain
Posted by: whiteheadtorut1996.blogspot.com


0 Response to "Can Swallowing A Can Tab Kill You"
Post a Comment